The Top Hormone Imbalances I See in Women

Hormones don’t fail quietly.
They speak through symptoms, often long before labs look “abnormal.”
In my clinical work, these are the most common hormone imbalances I see in women, especially during premenopause, perimenopause, and menopause. Many women experience more than one at the same time, which is why symptoms can feel confusing or contradictory.
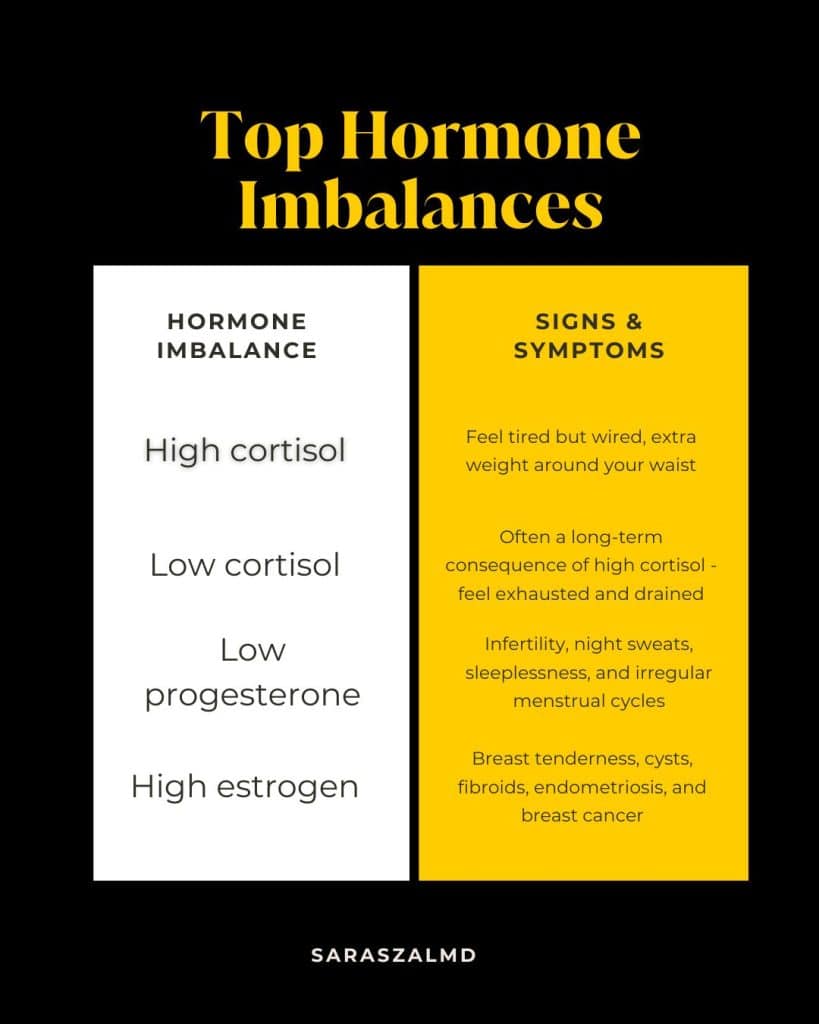
High Cortisol
Often driven by chronic stress or long-term overactivation of the stress response.
Common signs include:
Feeling tired but wired, difficulty sleeping, anxiety, and increased fat around the waist
Low Cortisol
Frequently a later-stage consequence of prolonged high cortisol.
Common signs include:
Persistent exhaustion, low stamina, feeling drained or depleted, and difficulty recovering from stress.
Low Progesterone
Often one of the earliest hormone shifts in the late 30s and 40s.
Common signs include:
Sleep disruption, night sweats, fertility challenges, PMS, and irregular menstrual cycles.
High Estrogen (Estrogen Dominance)
Can occur even when estrogen levels are “normal,” especially if progesterone is low or detoxification is impaired.
Common signs include:
Breast tenderness, cysts, fibroids, endometriosis, and increased risk patterns for breast disease.
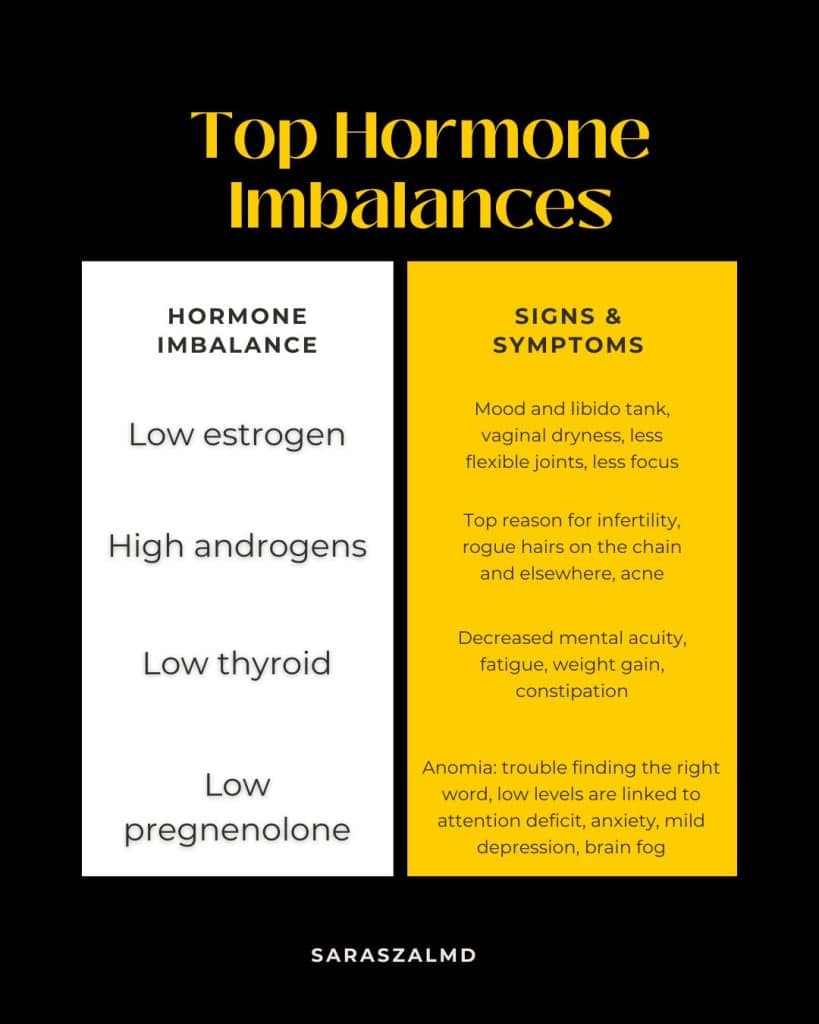
Low Estrogen
More common later in the menopausal transition, though it can appear earlier.
Common signs include:
Low mood and libido, vaginal dryness, decreased joint flexibility, reduced focus, and cognitive slowing.
High Androgens
Often linked to insulin resistance or ovarian/adrenal imbalance.
Common signs include:
Acne, excess facial or body hair (especially along the chin or jawline), and fertility challenges.
Low Thyroid Function
May be overt or subclinical and frequently overlaps with adrenal and insulin issues.
Common signs include:
Fatigue, weight gain, constipation, hair thinning, cold intolerance, and decreased mental clarity.
Low Pregnenolone
An underrecognized but critical hormone, especially for brain health.
Common signs include:
Word-finding difficulty, brain fog, attention challenges, anxiety, mild depression, and reduced cognitive resilience.
Here’s the good news: It is easier to rebalance your hormones than to live with the misery of hormonal imbalance. I have helped many women transform hormonal problems using simple yet powerful techniques.
You don’t need to settle for anything less than feeling fully alive and joyous before, during, and after midlife.
In my books, I use the best evidence to help you discover the root cause of hormone imbalance. Then I apply a science-based correction for this imbalance.
I leverage whatever it takes: nutrition, botanical remedies, critical precursors (essential ingredients to make brain chemicals and hormones) such as amino acids and B vitamins, ancient methodology, and bioidentical hormones.
More often than not, women have more than one hormonal imbalance.
If you believe your hormones are out of whack, where do you begin?
Chapter 1 in THE HORMONE CURE has a 7-part questionnaire that identifies the most common hormonal problems that can occur during premenopause, perimenopause, and menopause. That’s a great place to start.
What about andonomysis? thickening of the uterus and I just had mirena put in last march because of the bleeding and hoping to thin the lining. I also have low estrogen and progesterone.
Doctor don’t suggest to take estrogen because of my symptoms. I have lots difficulty with sleep, weight gain and anxiety. I started taking progesterone 100mg. I wanted to know what else can I take?
I hear how much you’re struggling, and I want you to know that your anxiety and lack of sleep are real biological signals. Managing adenomyosis alongside these hormonal shifts is incredibly taxing on your system, and I have adenomyosis myself. Because your situation involves specific prescriptions and a delicate balance with estrogen and progesterone, it’s so important to bring these concerns back to your doctor. They can look at your labs to see what’s safe to add next. You deserve to feel like yourself again, and getting that personalized clinical guidance is the best way to get there. Unfortunately I cannot give medical advice online, but my next book will address adenomyosis!!